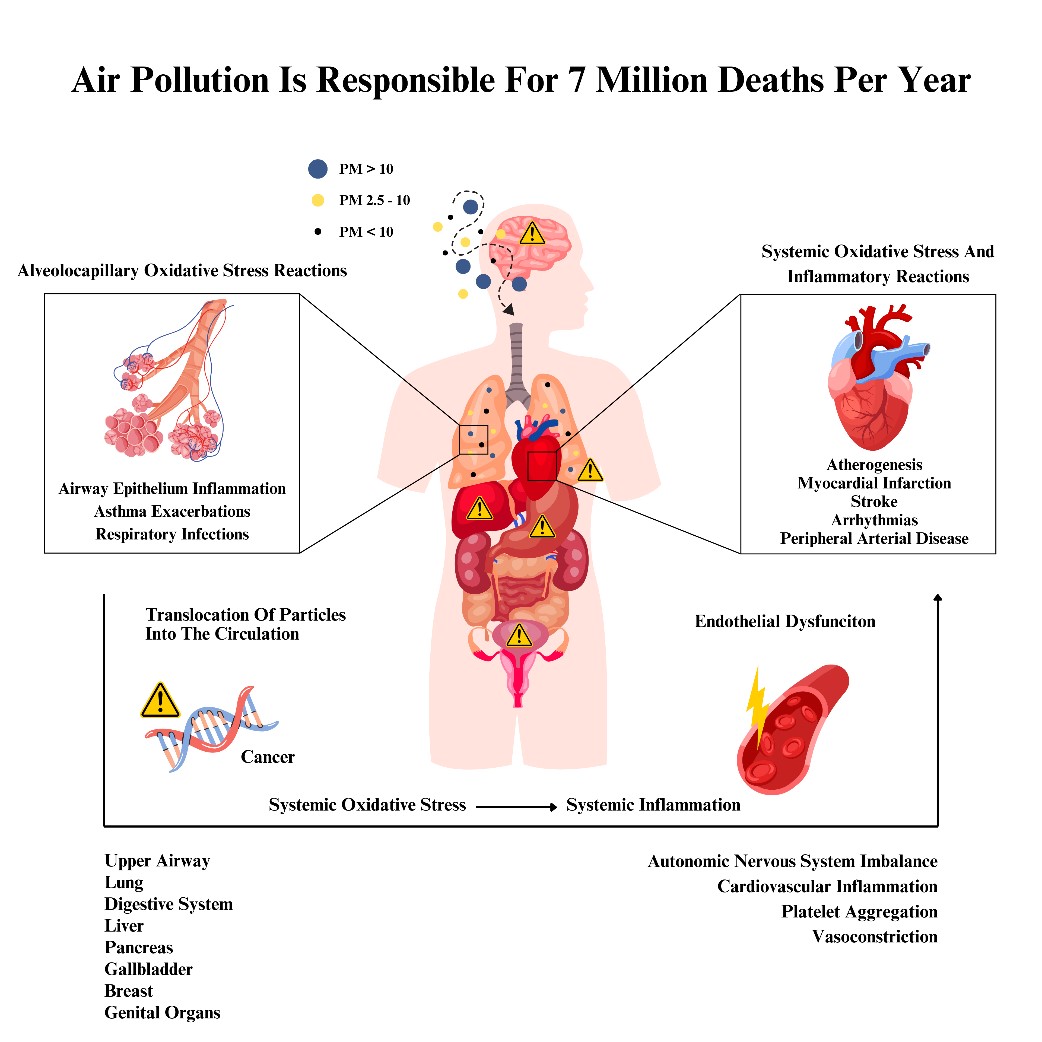
The movement and extent of penetration of particulate matter (PM) into the respiratory and circulatory systems are influenced by their size categories. Larger particles, such as PM10, predominantly impact the upper respiratory tract, whereas PM2.5 can infiltrate both the upper and lower respiratory tracts and enter the circulatory system, directly affecting health and increasing the risk of diseases. The ability of PM to carry harmful substances into the lungs is determined by factors such as particle density, size, shape, airway structure, and breathing patterns. Recent studies highlight that atmospheric PM with a diameter of less than 2.5 micrometers (PM2.5) is a critical environmental pollutant and the most significant contributor to the global disease burden. In urban areas worldwide, premature deaths linked to PM2.5 exposure range from 3 to 125 per 100,000 people [2-5].
Over half of these deaths are associated with elevated mortality rates from cardiovascular diseases (CVDs), including ischemic heart disease, cardiac arrhythmias, heart failure, and hypertension. Prolonged exposure to PM2.5 intensifies these risks, especially among vulnerable groups such as those with pre-existing conditions (e.g., diabetes mellitus, asthma, chronic obstructive pulmonary disease etc.), low-income communities, racial and ethnic minorities, and older adults [3-6]. This is particularly alarming, as only 8% of the world’s 250 largest cities have population-weighted average PM2.5 concentrations that meet the World Health Organization’s (WHO) recommended annual guidelines [1-6].
Air pollution stems from both natural sources (e.g., volcanoes, wildfires) and anthropogenic activities (e.g., fuel combustion, industrial processes, power generation, and agriculture). The latter is far more dominant due to its connection to economic globalization and industrialization [1,6]. CRB, the practice of incinerating agricultural waste to clear fields for the next crop cycle [7], contributes significantly to air pollution. Its impact varies by season, location, and agricultural practices and has been extensively documented in Southeast Asia [8]. India, as the world’s second-largest agrarian economy, generates substantial agricultural waste, much of which is routinely burned [9].
While extensive research has explored the harmful effects of air pollution, a detailed analysis of the health impacts specifically attributable to CRB, along with potential solutions, remains limited. This review emphasizes the significance of CRB as a major contributor to air pollution, aiming to inform policy-making in India and enhance sustainability and child flourishing indices for future generations.
Methods
To perform this narrative review, we leaned on published national and international data to individualize the health implications of CRB in India. The terms “crop residue burning”, “health effects”, “air pollution”, “India”, or any combination of them, were entered into Google Scholar and PubMed. Selected data coming from renowned international organizations was also utilized to complement the analysis.
Observations and Discussion
CRB in India and the related Health outcomes
CRB Situation in India
India contributes to 3.36% of the world's total GDP and 18% of it comes from agriculture. This sector is the backbone of Indian economy as it employs half of the country's body of work [10-12]. The productive nature of agriculture carries tremendous amounts of crop residues (~500 million tons (MT)/year), primarily from rice, wheat, maize, millet and sugarcane [9].
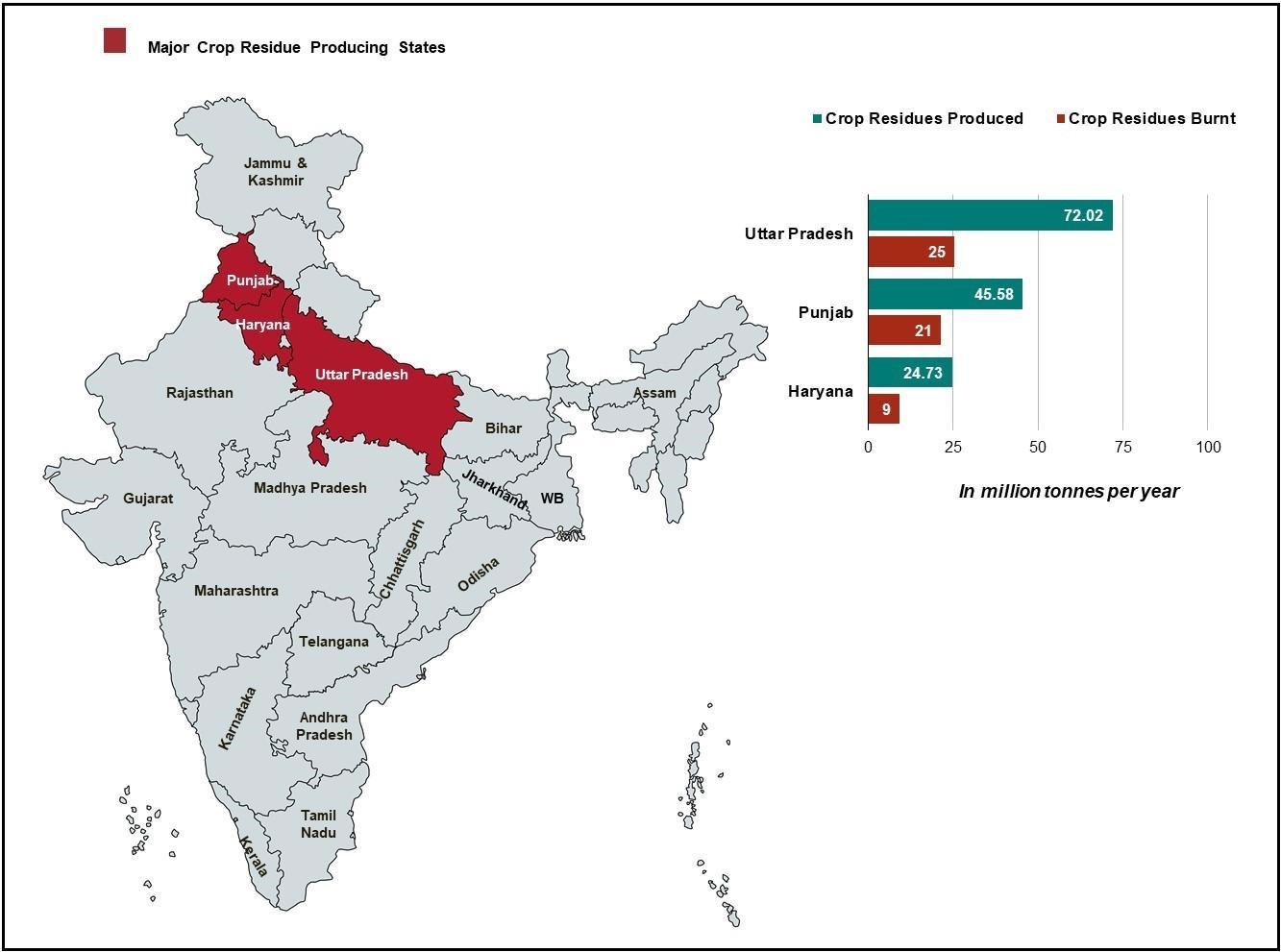
Agricultural residues are rich in minerals (e.g., zinc, copper, iron) and organic matter, that can aid in enhancing land fertility. It can also be converted into alternative energy (e.g., biofuel), and cattle fodder as it improves its overall health and milk production [13,14]. Nonetheless, CRB is seen as a more convenient approach than proper stubble management, as the latter can be expensive and time-consuming [15]. Approximately 25% of agricultural waste is burned to clear fields for the subsequent cereal crop, a practice particularly prevalent in Uttar Pradesh (~72.02 MT/year), Punjab (~45.58 MT/year) and Haryana (~24.73 MT/year) in Northwestern India ( Figure 1) [8,16].