Abstract
Background
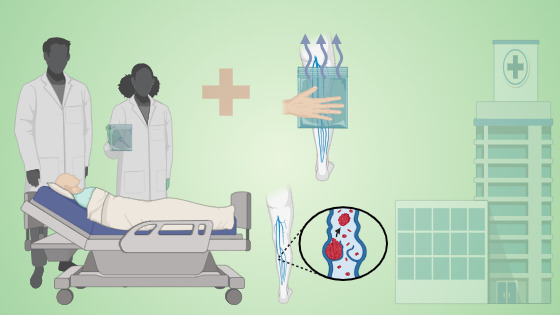
Thrombophlebitis is recognized as a potential complication of intravenous therapy. Treatment typically involves discontinuing the infusion line. Initially, a cold compress is applied to reduce blood flow and promote platelet aggregation. Subsequently, a warm compress is used. Elevating the affected extremity and relocating the intravenous line to the opposite extremity are also recommended. The present study analysed the efficacy of warm compression in patients with thrombophlebitis.
Methods
Present study was conducted among 50 thrombophlebitis patients at MCH-SKIMS, Bemina Srinagar. The sample for the present study were selected by non-probability convenience sampling technique. We utilized a standardized Visual Infusion Phlebitis scale for data collection. Subsequently, the collected data was analysed using paired-sample t-test to compare pre- and post-intervention scores using SPSS version 20.
Results
The study revealed that participants were predominantly aged 31-50 years (74%), with males comprising 56% and females 44%. Habits included 30% smokers, no alcohol consumers, 28% tobacco users, and 42% without harmful habits. Cannula duration varied: <2 days (18%), 2-3 days (36%), 3-5 days (30%), and 5 days (16%). Medication frequency was once daily (10%), twice daily (52%), thrice daily (32%), and every four hours (6%). Cannula sizes were 18 G (40%), 20 G (54%), and 22 G (6%). Pre-intervention thrombophlebitis mean score was 2.74 ± 1.337, reducing significantly post-intervention to 1.1 ± 1.055 (p < 0.0001), affirming the efficacy of warm compression in reducing thrombophlebitis severity.
Conclusion
In conclusion, nurses are pivotal in promoting patient health, especially in managing complications like thrombophlebitis during intravenous therapy. This study confirms that warm compression effectively reduces thrombophlebitis severity in patients. Significant differences in thrombophlebitis scores before and after warm compression demonstrate its clinical effectiveness.
Keywords:
Intravenous therapy, thrombophlebitis, warm compression, infusion therapy, nursing interventions, clinical effectivenessReferences
Deka J, Dutta A. A study to assess the effect of hot fomentation on thrombophlebitis among patients undergoing intravenous therapy admitted in the selected hospitals of Guwahati, Assam. IP Journal of Paediatrics and Nursing Science. 2022;5(2):55-61.
Sivakami S. A study to assess the effectiveness of hot fomentation on thrombophlebitis among patients received intravenous therapy at selected hospitals Tittagudi [Internet] . Thanthai Roever College of Nursing, Perambalur 2015. [cited on 2024 Oct 18]. Available from: http://repository-tnmgrmu.ac.in/2858/
Infusion Nurses Society. Setting the standard for infusion care. 2021;44:1.
Blessly Pramila SP. A study to evaluate the effectiveness of hot compress in reducing the signs and symptoms of phlebitis among toddlers with IV infusion therapy in a selected hospital at Coimbatore [Internet]. Annai Meenakshi College of Nursing, Coimbatore; 2012. [cited 2023 Oct 18]. Available from: http://repositorytnmgrmu.ac.in/3658/
Amin N, Naik S. Phlebitis prevention protocol. JMS. 2023;26(1):50-6.
Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. Brunner & Suddarth’s textbook of medical-surgical nursing. New Delhi: Lippincott Williams & Wilkins; 2010. p 308-17.
Patel R. Effect of Aloe vera gel in reducing pain and severity of inflammation among thrombophlebitis patients. Int J Recent Sci Res. 2019;10(12):36335-9.
Togalakis V, Kahn SR, Libman M, Blostein M. The epidemiology of peripheral vein infusion thrombophlebitis: a critical review. Am J Med. 2002 Aug;113(2):146-51.
Singh AK, Dwivedi R. Risk factors of thrombophlebitis at infusion sites in patients admitted in surgical ward: a prospective observational study. Int Surg J. 2018 May;5(5):1781-4.
Saji J, Korula SV, Mathew A, Mohan L. The incidence of thrombophlebitis following the use of peripheral intravenous cannula in post-operative patients: a prospective observational study. IOSR J Dent Med Sci. 2015;14(6):1-4.
Potter PA, Perry AG. Fundamentals of Nursing. Mosby Elsevier 2009 [Internet]. [cited on 2024 Oct 18]. Available from: https://www.worldcat.org/title/fundamentalsof-nursing/oclc/217277370
Smith PE. Clinical Nursing Skills. Lippincott Williams & Wilkins. 2005; 1-1010.
Guanche-Sicilia A, Begoña M, Elisa M, Ángel J, Gómez-Salgado J, Duarte-Clíments G. Prevention and treatment of phlebitis secondary to the insertion of a peripheral venous catheter: a scoping review from a nursing perspective. Healthcare (Basel). 2021 9(5):611
Aksoy F and Bayram SB 2023. The effect of warm moist compresses in peripheral intravenous catheter-related phlebitis. Eur J Oncol Nurs. 2023;67:102438.
Hankins J. Infusion therapy in clinical practice. The Infusion Nurses Society. 2001:394-5.
Kulisch Á, Bender T, Németh A and Szekeres L 2009. Effect of thermal water and adjunctive electrotherapy on chronic low back pain: A double-blind, randomized, follow up study. J Rehabil Med. 2009;41(1):73–79.
How to Cite
License
Copyright (c) 2024 Foziya Manzoor, Seerat Mohi-u-din, Asiya Jan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright© by the author(s). Published by the Evidence Journals. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.