Abstract
Background: Cardiac arrest during pregnancy is a serious condition that can cause significant morbidity and mortality for both the mother and the unborn child
Objective: This systematic review and meta-analysis seek to estimate the worldwide prevalence of cardiac arrest during pregnancy.
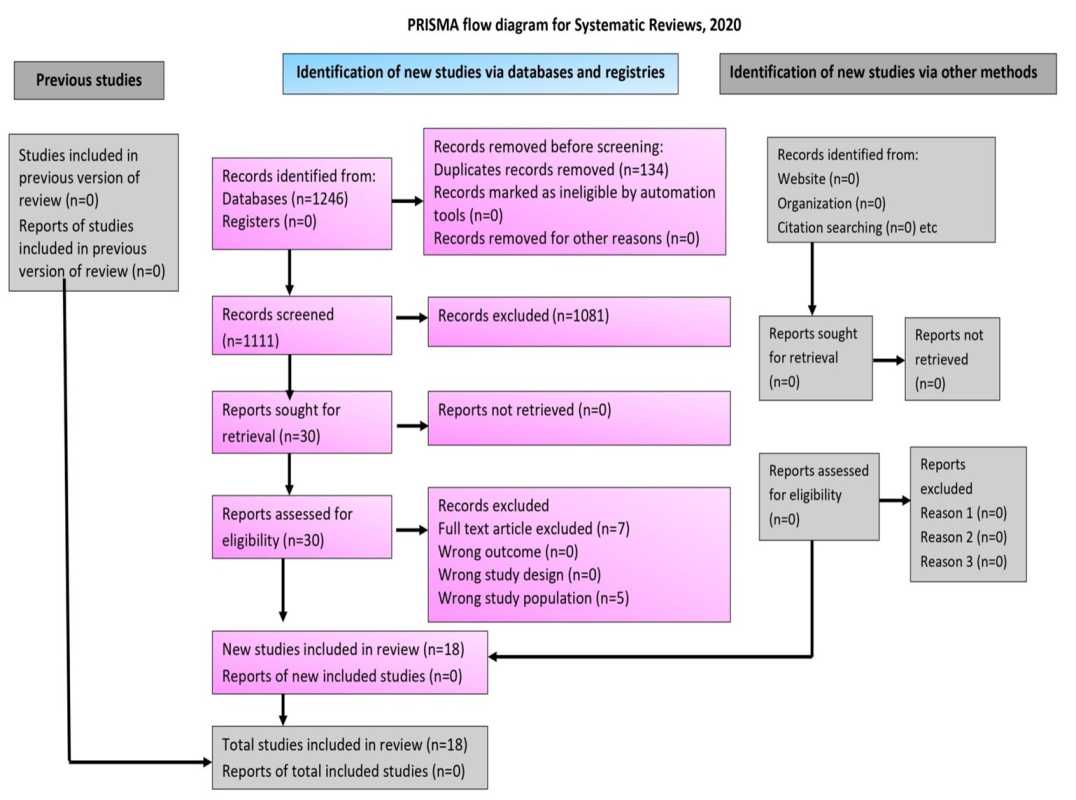
Methods: Multiple databases, including "PubMed, Cochrane, and Embase", were searched until April 7, 2023, exclusively in English, to ensure a comprehensive selection of relevant studies. A stringent two-stage screening process was employed, evaluating titles, abstracts, and full-text reviews based on the research question, "What is the prevalence of cardiac arrest in women during pregnancy?" Two authors independently extracted relevant data from the selected studies, including author names, publication years, study design, cardiac arrest occurrences, and total number of pregnant participants. The third author resolved the conflict. The Random Effects Model (REM) computed the pooled cardiac arrest prevalence. Heterogeneity was assessed via the I2 statistic.
Results: The systematic search of the database resulted in the identification of 1246 articles. Out of these, 18 were deemed suitable for inclusion in the systematic review, and ultimately, 17 of them were included in the meta-analysis.The pooled cardiac arrest prevalence during pregnancy was estimated at 0.08% (95% CI 0.03-0.19). The PI was <0.001-5.03%. However, the heterogeneity remained high (I2=100%). Sub-group analysis disclosed varying prevalence across continents, with Asia displaying the highest rate [(2.76%) (95% CI 1.04-7.12].
Conclusions: The study reveals significant cardiac arrest prevalence in pregnancy, with increasing rates over time and variations by continent. Maternal mortality concerns persist, particularly in Asia.
Keywords:
Cardiac arrest, Maternal mortality, Meta-analysis, Pregnancy, Cardiovascular disease, Antenatal, Intrapartum, Myocardial infarction, Angina, Evidence synthesisReferences
Knight M, Kenyon S, Brocklehurst P, Neilson JP, Shakespeare J, Kurinczuk JJ. Saving Lives, Improving Mothers' Care: Lessons learned to inform future maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-2012. In 2014.
Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet (London, England). 2006 Apr;367(9516):1066–74.
Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet (London, England). 2016 Jan;387(10017):462–74.
Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, Cifkova R, Ferreira R, Foidart JM, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011 Dec;32(24):3147–97.
Nair M, Nelson-Piercy C, Knight M. Indirect maternal deaths: UK and global perspectives. Obstet Med [Internet]. 2017 Feb 1;10(1):10–5. Available from: https://doi.org/10.1177/1753495X16689444
Storm F, Agampodi S, Eddleston M, Sørensen JB, Konradsen F, Rheinländer T. Indirect causes of maternal death. Vol. 2, The Lancet. Global health. England; 2014. p. e566.
Drenthen W, Boersma E, Balci A, Moons P, Roos-Hesselink JW, Mulder BJM, et al. Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J. 2010 Sep;31(17):2124–32.
Silversides CK, Grewal J, Mason J, Sermer M, Kiess M, Rychel V, et al. Pregnancy Outcomes in Women With Heart Disease: The CARPREG II Study. J Am Coll Cardiol. 2018 May;71(21):2419–30.
Roos-Hesselink JW, Ruys TPE, Stein JI, Thilén U, Webb GD, Niwa K, et al. Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. Eur Heart J. 2013 Mar;34(9):657–65.
Zaharatos J, St Pierre A, Cornell A, Pasalic E, Goodman D. Building U.S. Capacity to Review and Prevent Maternal Deaths. J Womens Health (Larchmt). 2018 Jan;27(1):1–5.
Jeejeebhoy FM, Zelop CM, Lipman S, Carvalho B, Joglar J, Mhyre JM, et al. Cardiac Arrest in Pregnancy: A Scientific Statement From the American Heart Association. Circulation. 2015 Nov;132(18):1747–73.
R G, Mahalingam S, K A, Goel K, Devendiran A. Pregnancy With Cardiac Arrest in the Emergency Department: Case Report With Review of Literature. Vol. 13, Cureus. United States; 2021. p. e14148.
Jeejeebhoy FM, Zelop CM, Lipman S, Carvalho B, Joglar J, Mhyre JM, et al. Cardiac Arrest in Pregnancy. Circulation [Internet]. 2015 Nov 3;132(18):1747–73. Available from: https://doi.org/10.1161/CIR.0000000000000300
Benson MD, Padovano A, Bourjeily G, Zhou Y. Maternal collapse: Challenging the four-minute rule. EBioMedicine. 2016 Apr;6:253–7.
Severe Maternal Morbidity in the United States | Pregnancy | Reproductive Health |CDC [Internet]. [cited 2023 May 8]. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html
Targets of Sustainable Development Goal 3 [Internet]. Available from: https://www.who.int/europe/about-us/our-work/sustainable-development-goals/targets-of-sustainable-development-goal-3
Mhyre JM, Tsen LC, Einav S, Kuklina E V, Leffert LR, Bateman BT. Cardiac arrest during hospitalisation for delivery in the United States, 1998-2011. Anesthesiology. 2014 Apr;120(4):810–8.
Balki M, Liu S, León JA, Baghirzada L. Epidemiology of Cardiac Arrest During Hospitalisation for Delivery in Canada: A Nationwide Study. Anesth Analg. 2017 Mar;124(3):890–7.
Beckett VA, Knight M, Sharpe P. The CAPS Study: incidence, management and outcomes of cardiac arrest in pregnancy in the UK: a prospective, descriptive study. BJOG. 2017 Aug;124(9):1374–81.
Schaap TP, Overtoom E, van den Akker T, Zwart JJ, van Roosmalen J, Bloemenkamp KWM. Maternal cardiac arrest in the Netherlands: A nationwide surveillance study. Eur J Obstet Gynecol Reprod Biol. 2019 Jun 1;237:145–50.
Ford ND, DeSisto CL, Galang RR, Kuklina E V, Sperling LS, Ko JY. Cardiac Arrest During Delivery Hospitalisation : A Cohort Study. Ann Intern Med. 2023 Mar;
Nivatpumin P, Lertbunnaphong T, Dittharuk D. A ten-year retrospective review of maternal cardiac arrest: Incidence, characteristics, causes, and outcomes in a tertiary-care hospital in a developing country. Taiwan J Obstet Gynecol. 2021 Nov;60(6):999–1004.
Cardiac Arrest Rates in Pregnancy Might Be Higher Than Expected. JAMA. 2023 Mar;
Jeejeebhoy FM, Zelop CM, Windrim R, Carvalho JCA, Dorian P, Morrison LJ. Management of cardiac arrest in pregnancy: a systematic review. Resuscitation. 2011 Jul;82(7):801–9.
Katsuragi S, Tanaka H, Hasegawa J, Nakamura M, Kanayama N, Nakata M, et al. Analysis of preventability of hypertensive disorder in pregnancy-related maternal death using the nationwide registration system of maternal deaths in Japan. J Matern neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2019 Oct;32(20):3420–6.
Rivera FB, Magalong JV, Tantengco OA, Mangubat GF, Villafuerte MG, Volgman AS. Maternal and neonatal outcomes among pregnant women with cardiovascular disease in the Philippines: a retrospective cross-sectional study from 2015-2019. J Matern neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2022 Dec;35(25):9922–33.
Köcher L, Rossides M, Remaeus K, Grunewald J, Eklund A, Kullberg S AE. Maternal and infant outcomes in sarcoidosis pregnancy: a Swedish population-based cohort study of first births. Respir Res. 2020 Aug;21(1):225.
Justin Paul G, Anne Princy S, Anju S, Anita S, Cecily Mary M, Gnanavelu G, et al. Pregnancy outcomes in women with heart disease: the Madras Medical College Pregnancy And Cardiac (M-PAC) Registry from India. Eur Heart J [Internet]. 2023 May 1;44(17):1530–40. Available from: https://doi.org/10.1093/eurheartj/ehad003
Enomoto N, Yamashita T, Furuta M, Tanaka H, Ng ESW, Matsunaga S, et al. Effect of maternal positioning during cardiopulmonary resuscitation: a systematic review and meta-analyses. BMC Pregnancy Childbirth. 2022 Feb;22(1):159.
Garg J, Shah K, Shah S, Turagam MK, Natale A, Lakkireddy D. Implantable cardioverter-defibrillator in patients with spontaneous coronary artery dissection presenting with sudden cardiac arrest. J Cardiovasc Electrophysiol. 2021 Sep;32(9):2595–600.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015 Sep;13(3):147–53.
Gandhi AP, Satapathy P, Rustagi S, Hermis AH, Sah R, Padhi BK. Comments on "Shigellosis in Southeast Asia: A systematic review and meta-analysis". Vol. 54, Travel medicine and infectious disease. Netherlands; 2023. p. 102593.
Li JM, Nguyen C, Joglar JA, Hamdan MH, Page RL. Frequency and outcome of arrhythmias complicating admission during pregnancy: experience from a high-volume and ethnically-diverse obstetric service. Clin Cardiol. 2008 Nov;31(11):538–41.
Lipczyńska M, Janisz K, Szymański P, Biernacka EK, Hanus-Durlej K, Dȩbska M, et al. Pregnancy-related cardiac non-elective hospitalisations and pregnancy outcomes. A tertiary referral cardiac center experience. Kardiol Pol [Internet]. 2021;79(8):789–95. Available from: https://www.embase.com/search/results?subaction=viewrecord&id=L2014627478&from=export
Kumar N, Yadav A. Perinatal outcome in women with hypertensive disorders of pregnancy in rural tertiary center of Northern India: A retrospective cohort study". Curr Pediatr Rev [Internet]. 2020;16(1):71–8. Available from: https://www.embase.com/search/results?subaction=viewrecord&id=L2004325183&from=export
Ballali S, Belkadi K, Assaidi A, Moussaid I, Salmi S, Habbal R. Prognosis of pregnancies complicated with arrhythmia in Morocco. Arch Cardiovasc Dis Suppl [Internet]. 2018;10(1):100. Available from: https://www.embase.com/search/results?subaction=viewrecord&id=L620309229&from=export
Lima F V, Koutrolou-Sotiropoulou P, Yen TYM, Stergiopoulos K. Clinical characteristics and outcomes in pregnant women with Ebstein anomaly at the time of delivery in the USA: 2003-2012. Arch Cardiovasc Dis [Internet]. 2016;109(6–7):390–8. Available from: https://www.embase.com/search/results?subaction=viewrecord&id=L609742255&from=export
Liu H, Huang TT, Lin JH. Risk factors and risk index of cardiac events in pregnant women with heart disease. Chin Med J (Engl). 2012 Oct;125(19):3410–5.
Balint OH, Siu SC, Mason J, Grewal J, Wald R, Oechslin EN, et al. Cardiac outcomes after pregnancy in women with congenital heart disease. Heart [Internet]. 2010;96(20):1656–61. Available from: https://www.embase.com/search/results?subaction=viewrecord&id=L359851584&from=export
Heemelaar S, Agapitus N, van den Akker T, Stekelenburg J, Mackenzie S, Hugo-Hamman C, et al. Experiences of a dedicated Heart and Maternal Health Service providing multidisciplinary care to pregnant women with cardiac disease in a tertiary centre in Namibia. Trop Med Int Heal [Internet]. 2022;27(9):803–14. Available from: https://www.embase.com/search/results?subaction=viewrecord&id=L2018685515&from=export
Lopez JL, Duarte G, Acosta Rullan JM, Obaed NG, Karpel D, Sekulits A, et al. The Effect of Admission During the Weekend On In-Hospital Outcomes for Patients With Peripartum Cardiomyopathy. Cureus. 2022 Nov;14(11):e31401.
Marschner S, von Huben A, Zaman S, Reynolds HR, Lee V, Choudhary P, et al. Pregnancy-related cardiovascular conditions and outcomes in a United States Medicaid population. Heart. 2022 Sep;108(19):1524–9.
Pfaller B, Dave Javier A, Grewal J, Gabarin N, Colman J, Kiess M, et al. Risk Associated With Valvular Regurgitation During Pregnancy. J Am Coll Cardiol. 2021 Jun;77(21):2656–64.
Köcher L, Rossides M, Remaeus K, Grunewald J, Eklund A, Kullberg S, et al. Maternal and infant outcomes in sarcoidosis pregnancy: a Swedish population-based cohort study of first births. Respir Res. 2020 Aug;21(1):225.
Dongarwar D, Taylor J, Ajewole V, Anene N, Omoyele O, Ogba C, et al. Trends in Appendicitis Among Pregnant Women, the Risk for Cardiac Arrest, and Maternal-Fetal Mortality. World J Surg. 2020 Dec;44(12):3999–4005.
Pierce-Williams RAM, Burd J, Felder L, Khoury R, Bernstein PS, Avila K, et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalised pregnancies: a United States cohort study. Am J Obstet Gynecol MFM. 2020 Aug;2(3):100134.
Easter SR, Rouse CE, Duarte V, Hynes JS, Singh MN, Landzberg MJ, et al. Planned vaginal delivery and cardiovascular morbidity in pregnant women with heart disease. Am J Obstet Gynecol. 2020 Jan;222(1):77.e1-77.e11.
Grotegut CA, Chisholm CA, Johnson LNC, Brown HL, Heine RP, James AH. Medical and obstetric complications among pregnant women aged 45 and older. PLoS One. 2014;9(4):e96237.
Pawar SJ, Anjankar VP, Anjankar A, Adnan M. Cardiopulmonary Arrest During Pregnancy: A Review Article. Cureus. 2023 Feb;15(2):e35219.
Kuklina E, Callaghan W. Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995-2006. BJOG. 2011 Feb;118(3):345–52.
Elkayam U, Goland S, Pieper PG, Silversides CK. High-Risk Cardiac Disease in Pregnancy: Part I. J Am Coll Cardiol [Internet]. 2016;68(4):396–410. Available from: https://www.sciencedirect.com/science/article/pii/S0735109716333526
Braund S, Leviel J, Morau E, Deneux-Tharaux C, Verspyck E. Maternal sudden death: A nationwide retrospective study. BJOG. 2023 Feb;130(3):257–63.
Kulkarni S, Futane SS. Cardiopulmonary Resuscitation in Obstetric Patient: Special Considerations. J Obstet Gynaecol India. 2022 Jun;72(3):192–200.
Thakkar A, Hameed AB, Makshood M, Gudenkauf B, Creanga AA, Malhamé I, et al. Assessment and Prediction of Cardiovascular Contributions to Severe Maternal Morbidity. JACC Adv [Internet]. 2023;2(2):100275. Available from: https://www.sciencedirect.com/science/article/pii/S2772963X23000297
Maternal mortality [Internet]. [cited 2023 May 2]. Available from: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
Isogai T, Kamiya CA. Worldwide Incidence of Peripartum Cardiomyopathy and Overall Maternal Mortality. Int Heart J. 2019 May;60(3):503–11.
Lewis G. Maternal mortality in the developing world: why do mothers really die? Obstet Med. 2008 Sep;1(1):2–6.
Girum T, Wasie A. Correlates of maternal mortality in developing countries: an ecological study in 82 countries. Matern Heal Neonatol Perinatol. 2017;3:19.
How to Cite
License
Copyright (c) 2023 The Evidence

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright© by the author(s). Published by the Evidence Journals. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.