Abstract
Background: The COVID-19 pandemic has had a profound impact on global health, revealing vulnerabilities in populations with pre-existing conditions. It has placed focus on the intersection of infectious diseases with chronic conditions, notably cardiovascular diseases. These have emerged as significant concerns due to their potential to exacerbate COVID-19 outcomes.
Objective: To estimate the prevalence of coronary artery disease (CAD) among COVID-19 patients.
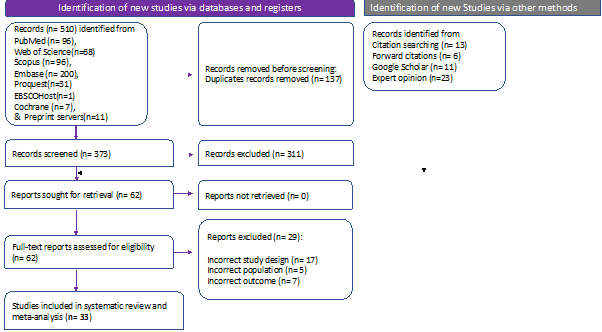
Methods: In this systematic review and meta-analysis, an extensive literature search was conducted in seven databases and preprint servers till 2023-04-13 as per a pre-registered protocol (CRD42022367501). Primary studies reporting CAD among COVID-19 patients were included. Individual study estimates were pooled using the random-effects model due to the heterogeneity. Prediction interval was used to identify the range into which future studies are expected to fall. Subgroup analysis and meta-regression were done to reduce heterogeneity, followed by publication bias and quality assessments.
Results: 33 studies with 40,064 COVID-19 patients revelaed a pooled prevalence of coronary artery disease of 15.24% (95% CI: 11.41% - 20.06%). The 95% prediction interval ranged from 2.49% to 55.90%. The studies were highly heterogeneous (tau-sqaured=0.89), and subgroup analysis significantly reduced it (P=.002). Europe reported the highest prevalence [21.70% (14.80% - 30.65%)], and Asia has the least prevalence [10.07% (6.55% - 15.19%)]. A symmetric doi plot and an LFK index of 0.57 revealed no evidence of publication bias.
Conclusions: The substantial prevalence of CAD among COVID-19 patients underscores the need for high clinical vigilance. The geographical disparities suggest potential regional differences in healthcare infrastructure, genetic predispositions, or lifestyle factors that warrant further investigation. The findings emphasize the importance of routine cardiac assessments for COVID-19 patients for timely interventions and better patient outcomes.
Keywords:
Coronary artery disease, COVID-19, Ischaemic heart disease, Myocardial infarction, Heart attack, Systematic Review, Meta-analysis, Angina pectoris, Coronavirus, Evidence synthesisReferences
Bansal M (2020) Cardiovascular disease and COVID-19. Diabetes Metab Syndr Clin Res Rev 14:247–250
World Health Organization (2023) WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int.
Bajgain KT, Badal S, Bajgain BB, Santana MJ (2021) Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. American Journal of Infection Control 49:238–246
Kumar R, Rai AK, Phukan MM, Hussain A, Borah D, Gogoi B, Chakraborty P, Buragohain AK (2021) Accumulating Impact of Smoking and Co-morbidities on Severity and Mortality of COVID-19 Infection: A Systematic Review and Meta-analysis. Curr Genomics 22:339–352
Carethers JM (2021) Insights into disparities observed with COVID‐19. J Intern Med 289:463–473
Ningthoujam R, Khomdram D (2020) WHO statement – “Older people are at highest risk from COVID-19”: Should the hypothesis be corroborated or rejected? Med Hypotheses. https://doi.org/10.1016/j.mehy.2020.109896
Barman HA, Atici A, Sahin I, et al (2021) Prognostic significance of cardiac injury in COVID-19 patients with and without coronary artery disease. Coronary Artery Disease 32:359
Harikrishnan S, Mohanan PP, Chopra VK, et al (2020) Cardiological society of India position statement on COVID-19 and heart failure. Indian Heart J 72:75–81
Kumar B, Kodliwadmath A, Upadhyay A, Singh A, N N (2021) Apparently normal epicardial coronaries in a patient with inferior wall myocardial infraction on the background of mild coronavirus disease-2019: take a second look! Monaldi Arch Chest Dis. https://doi.org/10.4081/monaldi.2021.1668
Ahlers MJ, Srivastava PK, Basir MB, O’Neill WW, Hacala M, Ammar K, Khalil S, Hollowed J, Nsair A (2022) Characteristics and outcomes of patients presenting with acute myocardial infarction and cardiogenic shock during COVID-19. Catheter Cardiovasc Interv 100:568–574
Yalamanchi R, Dasari BC, Narra L, Oomman A, Kumar P, Nayak R, Showkathali R (2020) Cardiac intensive care unit admissions during covid-19 pandemic—single center experience. Indian J Crit Care Med 24:1103–1105
Wang Z, Fu B, Lin Y, et al (2022) Red blood cell distribution width: A severity indicator in patients with COVID‐19. Journal of Medical Virology 94:2133–2138
Abe T, Egbuche O, Igwe J, Jegede O, Wagle B, Olanipekun T, Onwuanyi A (2021) Cardiovascular complications in COVID-19 patients with or without diabetes mellitus. Endocrinol Diabetes Metab. https://doi.org/10.1002/edm2.218
Choudhary R, Kaushik A, Sharma JB (2020) COVID-19 pandemic and stent thrombosis in a post percutaneous coronary intervention patient-a case report highlighting the selection of P2Y12 inhibitor. Cardiovasc Diagn Theer 10:898–901
Garg N, McClafferty B, Ramgobin D, Golamari R, Jain R, Jain R (2021) Cardiology and COVID-19: Do we have sufficient information? Future Cardiol 17:705–711
Stijnen T, Hamza TH, Ozdemir P (2010) Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Statistics in medicine 29:3046–67
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Statistics in medicine 21:1539–58
Shamim MA, Dwivedi P, Padhi BK (2023) Beyond the Funnel Plot: The Advantages of Doi Plots and Prediction Intervals in Meta-Analyses. Asian Journal of Psychiatry 103550–103550
Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, Kuss O, Higgins JPT, Langan D, Salanti G (2016) Methods to estimate the between-study variance and its uncertainty in meta-analysis. Research synthesis methods 7:55–79
Cochran WG (1954) The Combination of Estimates from Different Experiments. Biometrics 10:101–101
Aladağ N, Atabey RD (2021) The role of concomitant cardiovascular diseases and cardiac biomarkers for predicting mortality in critical COVID-19 patients. Acta Cardiologica 76:132–139
Argenziano MG, Bruce SL, Slater CL, et al (2020) Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ 369:m1996
Bali R, Calton RK (2021) Cardiovascular complications in COVID-19: A comparative study of clinical characteristics and their effect on the outcome of first wave and second wave. Indian Heart J 73:S66–S67
Bruce E, Barlow-Pay F, Short R, et al (2020) Prior Routine Use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and Important Outcomes in Hospitalised Patients with COVID-19. JCM 9:2586
Cen Y, Chen X, Shen Y, et al (2020) Risk factors for disease progression in patients with mild to moderate coronavirus disease 2019—a multi-centre observational study. Clinical Microbiology and Infection 26:1242–1247
Chen R, Liang W, Jiang M, et al (2020) Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China. CHEST 158:97–105
Deng Q, Hu B, Zhang Y, Wang H, Zhou X, Hu W, Cheng Y, Yan J, Ping H, Zhou Q (2020) Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. International Journal of Cardiology 311:116–121
Du Y, Tu L, Zhu P, et al (2020) Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan. A Retrospective Observational Study. Am J Respir Crit Care Med 201:1372–1379
Gupta N, Ish P, Kumar R, Dev N, Yadav SR, Malhotra N, Agrawal S, Gaind R, Sachdeva H, Group *Other members of the Safdarjung Hospital COVID 2019 working (2020) Evaluation of the clinical profile, laboratory parameters and outcome of two hundred COVID-19 patients from a tertiary centre in India. Monaldi Archives for Chest Disease. https://doi.org/10.4081/monaldi.2020.1507
Hewitt J, Carter B, Vilches-Moraga A, et al (2020) The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. The Lancet Public Health 5:e444–e451
Iaccarino G, Grassi G, Borghi C, et al (2020) Age and Multimorbidity Predict Death Among COVID-19 Patients. Hypertension 76:366–372
Inciardi RM, Adamo M, Lupi L, et al (2020) Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. European Heart Journal 41:1821–1829
Jamora RDG, Prado MB, Anlacan VMM, Sy MCC, Espiritu AI (2022) Incidence and risk factors for stroke in patients with COVID-19 in the Philippines: An analysis of 10,881 cases. Journal of Stroke and Cerebrovascular Diseases 31:106776
Lagi F, Piccica M, Graziani L, et al (2020) Early experience of an infectious and tropical diseases unit during the coronavirus disease (COVID-19) pandemic, Florence, Italy, February to March 2020. Eurosurveillance 25:2000556
Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, Vander K, Bargfrieder U, Trauner M (2020) Pulmonary Arterial Thrombosis in COVID-19 With Fatal Outcome. Ann Intern Med 173:350–361
Lendorf ME, Boisen MK, Kristensen PL, et al (2020) Characteristics and early outcomes of patients hospitalised for COVID-19 in North Zealand, Denmark. Dan Med J 67:A06200428
Li J, Xu G, Yu H, Peng X, Luo Y, Cao C (2020) Clinical Characteristics and Outcomes of 74 Patients With Severe or Critical COVID-19. The American Journal of the Medical Sciences 360:229–235
Liao Y, Feng Y, Wang B, et al (2020) Clinical characteristics and prognostic factors of COVID-19 patients progression to severe: a retrospective, observational study. Aging 12:18853–18865
Lodigiani C, Iapichino G, Carenzo L, et al (2020) Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thrombosis Research 191:9–14
Meloche C, Azam TU, Anderson E, et al (2021) CARDIOVASCULAR DISEASE AND OUTCOMES IN CRITICALLY ILL PATIENTS WITH COVID-19: A STOP-COVID ANCILLARY. J Am Coll Cardiol 77:3127
Prabhakaran D, Singh K, Kondal D, et al (2022) Cardiovascular Risk Factors and Clinical Outcomes among Patients Hospitalized with COVID-19: Findings from the World Heart Federation COVID-19 Study. Glo Heart. https://doi.org/10.5334/GH.1128
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, and the Northwell COVID-19 Research Consortium (2020) Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 323:2052–2059
Rossi PG, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R, Group the REC-19 W (2020) Characteristics and outcomes of a cohort of COVID-19 patients in the Province of Reggio Emilia, Italy. PLOS ONE 15:e0238281
Scoccia A, Gallone G, Cereda A, et al (2021) Impact of clinical and subclinical coronary artery disease as assessed by coronary artery calcium in COVID-19. Atherosclerosis 328:136–143
Shi S, Qin M, Cai Y, et al (2020) Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. European Heart Journal 41:2070–2079
Slipczuk L, Castagna F, Schonberger A, Novogrodsky E, Sekerak R, Dey D, Jorde UP, Levsky JM, Garcia MJ (2021) Coronary artery calcification and epicardial adipose tissue as independent predictors of mortality in COVID-19. Int J Cardiovasc Imaging 37:3093–3100
Tai S, Tang J, Yu B, et al (2020) Association between Cardiovascular Burden and Requirement of Intensive Care among Patients with Mild COVID-19. Cardiovascular Therapeutics 2020:e9059562
Turagam MK, Musikantow D, Goldman ME, et al (2020) Malignant Arrhythmias in Patients With COVID-19. Circulation: Arrhythmia and Electrophysiology 13:e008920
Xie Y, You Q, Wu C, Cao S, Qu G, Yan X, Han X, Wang C, Zhang H (2020) Impact of Cardiovascular Disease on Clinical Characteristics and Outcomes of Coronavirus Disease 2019 (COVID-19). Circ J 84:1277–1283
Xingwei H, Jinsheng L, Jia C, Mengwen W, Yujian L, Zhichao X, Chang X, Shusheng L, Hesong Z (2020) Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients. Chinese Journal of Cardiology 48:456–460
Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y, Akdis CA, Gao Y (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75:1730–1741
Zhang L, Feng X, Zhang D, et al (2020) Deep Vein Thrombosis in Hospitalized Patients With COVID-19 in Wuhan, China. Circulation 142:114–128
The World Health Organisation -COVID-19 Dashboard.
Benjamin EJ, Muntner P, Alonso A, et al (2019) Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 139:e56–e528
Townsend N WE CVD-statistics-report-August-2017.pdf.
Shi S, Qin M, Shen B, et al (2020) Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol 5:802–810
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z (2020) Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 5:811–818
Docea A, Tsatsakis A, Albulescu D, et al (2020) A new threat from an old enemy: Re‑emergence of coronavirus (Review). Int J Mol Med. https://doi.org/10.3892/ijmm.2020.4555
How to Cite
License
Copyright (c) 2023 The Evidence

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright© by the author(s). Published by the Evidence Journals. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Most read articles by the same author(s)
- Diptismita Jena, Prafulla Kumar Swain, Nandhni Chiruganam Gandhi, Visweswara Rao Guthi, Sree Sudha T Y, Priyadharshini. P, Sai Sreevalli Sreepada, Carlos Quispe- Vicuña, Mirza Adil Beig, Shilpa DM, Cancer burden and trends across India (1990-2021): insights from the Global Burden of Disease study , The Evidence: Vol. 2 No. 3 (2024): JUL - SEP