Abstract
Zoonotic diseases, exemplified by the recent COVID-19 pandemic, have posed significant threats to global public health. Among these, Nipah virus (NiV) stands out as a lethal pathogen responsible for outbreaks with high morbidity and mortality rates. This comprehensive review explores the clinical spectrum of NiV, focusing on epidemiology, transmission dynamics, clinical manifestations, diagnosis, treatment options, recent advancements in vaccine development, and mitigation strategies.
The epidemiology of NiV is characterized by its zoonotic nature, with fruit bats serving as natural reservoirs and various intermediate hosts facilitating transmission to humans and animals. Distinct outbreaks have occurred in different regions, with variations in transmission patterns and clinical outcomes. Clinical manifestations of NiV infection vary across species. In pigs, it leads to swine respiratory and neurological syndrome, while dogs and cats exhibit respiratory distress and renal dysfunction. In humans, NiV infection often manifests as acute encephalitis with diverse neurological symptoms, including sensory disturbances, myoclonus, and late-onset complications.
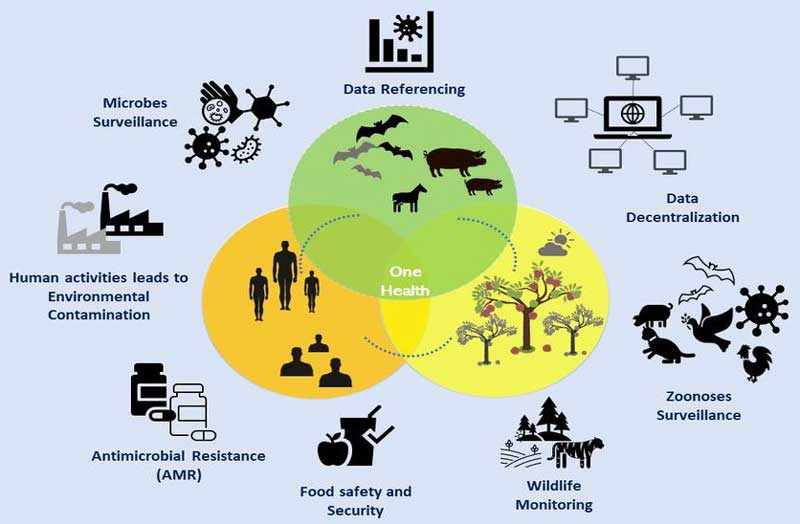
Diagnosis relies on a combination of assays, including RT-PCR, virus isolation, and antibody detection. Despite the absence of specific treatments, ribavirin and experimental therapies show promise in reducing mortality. Several NiV vaccine candidates are in development, with some showing efficacy in animal models. Prevention and mitigation strategies include livestock infection control, public awareness campaigns, infection prevention in healthcare settings, biosafety measures, and active surveillance. Climate change and human activities contribute to viral spillover, emphasizing the need for a One Health approach to manage NiV and other emerging infectious diseases.
Keywords:
nipah virus, zoonosis, one health, clinical spectrum, epidemiology, transmission, vaccine, mitigation strategiesReferences
Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, et al. Global trends in emerging infectious diseases. Nature [Internet]. 2008 Feb 21 [cited 2023 Sep 23];451(7181):990. Available from: /pmc/articles/PMC5960580/
Ang BSP, Lim TCC, Wang L. Nipah virus infection. J Clin Microbiol [Internet]. 2018 Jun 1 [cited 2023 Sep 20];56(6). Available from: https://journals.asm.org/doi/10.1128/jcm.01875-17
Angeletti S, Lo Presti A, Cella E, Ciccozzi M. Molecular epidemiology and phylogeny of Nipah virus infection: A mini review. Asian Pac J Trop Med. 2016 Jul 1;9(7):630–4.
WHO. Nipah virus [Internet]. 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/nipah-virus
Aljofan M. Hendra and Nipah infection: Emerging paramyxoviruses. Virus Res [Internet]. 2013 Nov;177(2):119–26. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168170213002657
Ksiazek TG, Rota PA, Rollin PE. A review of Nipah and Hendra viruses with an historical aside. Virus Res [Internet]. 2011 Dec [cited 2023 Sep 23];162(1–2):173–83. Available from: https://pubmed.ncbi.nlm.nih.gov/21963678/
Ksiazek TG, Rota PA, Rollin PE. A review of Nipah and Hendra viruses with an historical aside. Virus Res [Internet]. 2011 Dec;162(1–2):173–83. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168170211003790
Baranowski K, Bharti N. Habitat loss for black flying foxes and implications for Hendra virus. Landsc Ecol [Internet]. 2023 Jun 1 [cited 2023 Sep 23];38(6):1605–18. Available from: http://www.ncbi.nlm.nih.gov/pubmed/37229480
Mahalingam S, Herrero LJ, Playford EG, Spann K, Herring B, Rolph MS, et al. Hendra virus: an emerging paramyxovirus in Australia. Lancet Infect Dis [Internet]. 2012 Oct [cited 2023 Sep 23];12(10):799–807. Available from: https://pubmed.ncbi.nlm.nih.gov/22921953/
Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, et al. Nipah Virus-associated Encephalitis Outbreak, Siliguri, India. Emerg Infect Dis [Internet]. 2006 [cited 2023 Sep 23];12(2):235. Available from: /pmc/articles/PMC3373078/
Donna Lu and Agencies. What is Nipah virus? Kerala starts mass testing after outbreak in India. The Guardian [Internet]. 2023; Available from: https://www.theguardian.com/world/2023/sep/18/what-is-nipah-virus-kerala-india-bat-borne-outbreak-mass-testing
Devnath P, Masud HMAA. Nipah virus: a potential pandemic agent in the context of the current severe acute respiratory syndrome coronavirus 2 pandemic. New microbes new Infect [Internet]. 2021 May 1 [cited 2023 Sep 23];41. Available from: https://pubmed.ncbi.nlm.nih.gov/33758670/
Carrasco-Hernandez R, Jácome R, Vidal YL, de León SP. Are RNA Viruses Candidate Agents for the Next Global Pandemic? A Review. ILAR J [Internet]. 2017 Dec 15 [cited 2023 Sep 23];58(3):343–58. Available from: https://pubmed.ncbi.nlm.nih.gov/28985316/
Centers for Disease Control and Prevention (CDC). Update: outbreak of Nipah virus--Malaysia and Singapore, 1999. MMWR Morb Mortal Wkly Rep [Internet]. 1999 Apr 30 [cited 2023 Sep 23];48(16):335–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10366143
Banerjee S, Gupta N, Kodan P, Mittal A, Ray Y, Nischal N, et al. Nipah virus disease: A rare and intractable disease. Intractable Rare Dis Res [Internet]. 2019 [cited 2023 Sep 23];8(1):1. Available from: /pmc/articles/PMC6409114/
Nikolay B, Salje H, Hossain MJ, Khan AKMD, Sazzad HMS, Rahman M, et al. Transmission of Nipah Virus — 14 Years of Investigations in Bangladesh. N Engl J Med [Internet]. 2019 May 9;380(19):1804–14. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1805376
Clayton BA, Middleton D, Bergfeld J, Haining J, Arkinstall R, Wang L, et al. Transmission routes for nipah virus from Malaysia and Bangladesh. Emerg Infect Dis [Internet]. 2012 Dec [cited 2023 Sep 24];18(12):1983–93. Available from: https://pubmed.ncbi.nlm.nih.gov/23171621/
Mohd Nor MN, Gan CH, Ong BL. Nipah virus infection of pigs in peninsular Malaysia. Rev Sci Tech [Internet]. 2000 Apr [cited 2023 Sep 24];19(1):160–5. Available from: https://pubmed.ncbi.nlm.nih.gov/11189713/
THE STATUS, PUBLIC RESPONSE AND CHALLENGES IN OVERCOMING EMERGING AND EXOTIC DISEASES - NIPAH VIRUS DISEASE EXPERIENCE [Internet]. [cited 2023 Sep 24]. Available from: https://www.researchgate.net/publication/280224022_THE_STATUS_PUBLIC_RESPONSE_AND_CHALLENGES_IN_OVERCOMING_EMERGING_AND_EXOTIC_DISEASES_-_NIPAH_VIRUS_DISEASE_EXPERIENCE
Goh KJ, Tan CT, Chew NK, Tan PSK, Kamarulzaman A, Sarji SA, et al. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N Engl J Med [Internet]. 2000 Apr 27 [cited 2023 Sep 24];342(17):1229–35. Available from: https://pubmed.ncbi.nlm.nih.gov/10781618/
Ang BSP, Lim TCC, Wang L. Nipah Virus Infection. Kraft CS, editor. J Clin Microbiol [Internet]. 2018 Jun;56(6). Available from: https://journals.asm.org/doi/10.1128/JCM.01875-17
Abdullah, Suhailah; Li-Yen Chang; Rahmat KKJGCTT. Late-onset Nipah virus encephalitis 11 years after the initial outbreak: A case report. Neurol Asia [Internet]. 2012;17(1):71–4. Available from: https://web.s.ebscohost.com/abstract?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=18236138&asa=Y&AN=74271978&h=IGNiGWXMu6jf%2F7qRwOl7WUptIy5EM%2BAwxmkgiq7HRLJmmp0IBgY9TTPZHcM%2FYsecDIO%2FoNXnZgDcG4obqeC2EQ%3D%3D&crl=c&resultNs=AdminWebAuth&r
Ng BY, Lim CCT, Yeoh A, Lee WL. Neuropsychiatric Sequelae of Nipah Virus Encephalitis. J Neuropsychiatry Clin Neurosci [Internet]. 2004 Nov;16(4):500–4. Available from: http://psychiatryonline.org/doi/abs/10.1176/jnp.16.4.500
Daniels P, Ksiazek T, Eaton BT. Laboratory diagnosis of Nipah and Hendra virus infections. Microbes Infect [Internet]. 2001 [cited 2023 Sep 24];3(4):289–95. Available from: https://pubmed.ncbi.nlm.nih.gov/11334746/
Chong HT, Kamarulzaman A, Tan CT, Goh KJ, Thayaparan T, Kunjapan SR, et al. Treatment of acute Nipah encephalitis with ribavirin. Ann Neurol [Internet]. 2001 [cited 2023 Sep 25];49(6):810–3. Available from: https://pubmed.ncbi.nlm.nih.gov/11409437/
Bossart KN, Zhu Z, Middleton D, Klippel J, Crameri G, Bingham J, et al. A Neutralizing Human Monoclonal Antibody Protects against Lethal Disease in a New Ferret Model of Acute Nipah Virus Infection. PLOS Pathog [Internet]. 2009 Oct [cited 2023 Sep 25];5(10):e1000642. Available from: https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1000642
Aditi, Shariff M. Nipah virus infection: A review. Epidemiol Infect [Internet]. 2019 [cited 2023 Sep 25];147:e95. Available from: https://www.cambridge.org/core/journals/epidemiology-and-infection/article/nipah-virus-infection-a-review/4D3B54325AF2E6BB45C34E96EA71D66E
Devnath P, Masud HMAA. Nipah virus: a potential pandemic agent in the context of the current severe acute respiratory syndrome coronavirus 2 pandemic. New microbes new Infect [Internet]. 2021 May 1 [cited 2023 Sep 25];41. Available from: https://pubmed.ncbi.nlm.nih.gov/33758670/
Sayed A, Bottu A, Qaisar M, Mane MP, Acharya Y. Nipah virus: a narrative review of viral characteristics and epidemiological determinants. Public Health [Internet]. 2019 Aug 1 [cited 2023 Sep 25];173:97–104. Available from: https://pubmed.ncbi.nlm.nih.gov/31261032/
Ambat AS, Zubair SM, Prasad N, Pundir P, Rajwar E, Patil DS, et al. Nipah virus: A review on epidemiological characteristics and outbreaks to inform public health decision making. J Infect Public Health. 2019 Sep 1;12(5):634–9.
Soltan MA, Eldeen MA, Elbassiouny N, Mohamed I, El-damasy DA, Fayad E, et al. Proteome Based Approach Defines Candidates for Designing a Multitope Vaccine against the Nipah Virus. Int J Mol Sci [Internet]. 2021 Aug 28;22(17):9330. Available from: https://www.mdpi.com/1422-0067/22/17/9330
Satterfield BA. The future of preventing and treating Nipah virus infection. Futur Sci OA [Internet]. 2017 Nov;3(4):FSO220. Available from: https://www.future-science.com/doi/10.4155/fsoa-2017-0056
TEKOLA B, MYERS L, LUBROTH J, PLEE L, CALISTRI P, PINTO J. International health threats and global early warning and response mechanisms. Rev Sci Tech l’OIE [Internet]. 2017 Aug 1;36(2):657–70. Available from: https://doc.oie.int/dyn/portal/index.xhtml?page=alo&aloId=35336
Central Team, MoHFW G. Clinical Management Protocol for Nipah Viral Disease [Internet]. 2018. Available from: https://www.ncdc.gov.in/showfile.php?lid=241
Sharma V, Kaushik S, Kumar R, Yadav JP, Kaushik S. Emerging trends of Nipah virus: A review. Rev Med Virol [Internet]. 2019 Jan 1 [cited 2023 Sep 25];29(1). Available from: https://pubmed.ncbi.nlm.nih.gov/30251294/
Looi LM, Chua KB. Lessons from the Nipah virus outbreak in Malaysia. Malays J Pathol [Internet]. 2007 Dec;29(2):63–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19108397
Control. C for D. Outbreak of Hendra-like virus—Malaysia and Singapore, 1998–1999. MMWR Morb Mortal Wkly Rep. 1999;48:265–9.
Paton NI, Leo YS, Zaki SR, Auchus AP, Lee KE, Ling AE, et al. Outbreak of Nipah-virus infection among abattoir workers in Singapore. Lancet [Internet]. 1999 Oct 9 [cited 2023 Sep 23];354(9186):1253–6. Available from: http://www.thelancet.com/article/S0140673699043792/fulltext
Mahmudur Rahmana AC. Nipah virus outbreaks in Bangladesh: a deadly infectious disease. WHO South-East Asia J Public Heal. 2012;1(2):208–12.
MOHFW B. Ministry of Health & Family Welfare . Government of the People’s Republic of Bangladesh [Internet]. Available from: http://www.mohfw.gov.bd/
Luby SP, Rahman M, Hossain MJ, Blum LS, Husain MM, Gurley E, et al. Foodborne transmission of Nipah virus, Bangladesh. Emerg Infect Dis. 2006;12(12):1888–94.
Ching PKG, de los Reyes VC, Sucaldito MN, Tayag E, Columna-Vingno AB, Malbas FF, et al. Outbreak of Henipavirus Infection, Philippines, 2014. Emerg Infect Dis [Internet]. 2015 Feb;21(2):328–31. Available from: http://wwwnc.cdc.gov/eid/article/21/2/14-1433_article.htm
Nipah virus deaths reported in India | CIDRAP [Internet]. [cited 2023 Sep 23]. Available from: https://www.cidrap.umn.edu/nipah/nipah-virus-deaths-reported-india
Uwishema O, Wellington J, Berjaoui C, Muoka KO, Onyeaka CVP, Onyeaka H. A short communication of Nipah virus outbreak in India: An urgent rising concern. Ann Med Surg [Internet]. 2022 Oct;82. Available from: https://journals.lww.com/10.1016/j.amsu.2022.104599
How to Cite
License
Copyright (c) 2024 The Evidence

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright© by the author(s). Published by the Evidence Journals. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.