Introduction
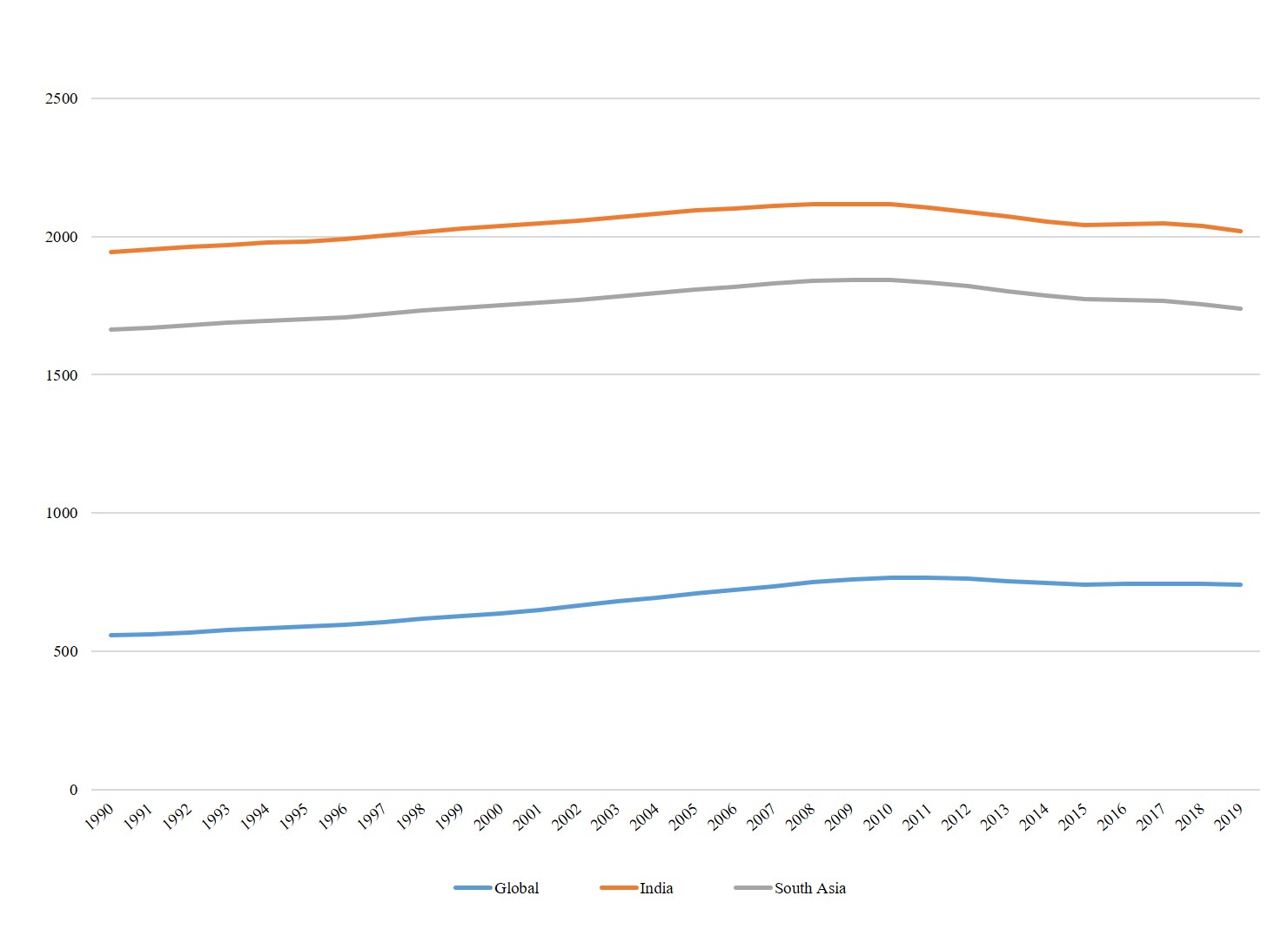
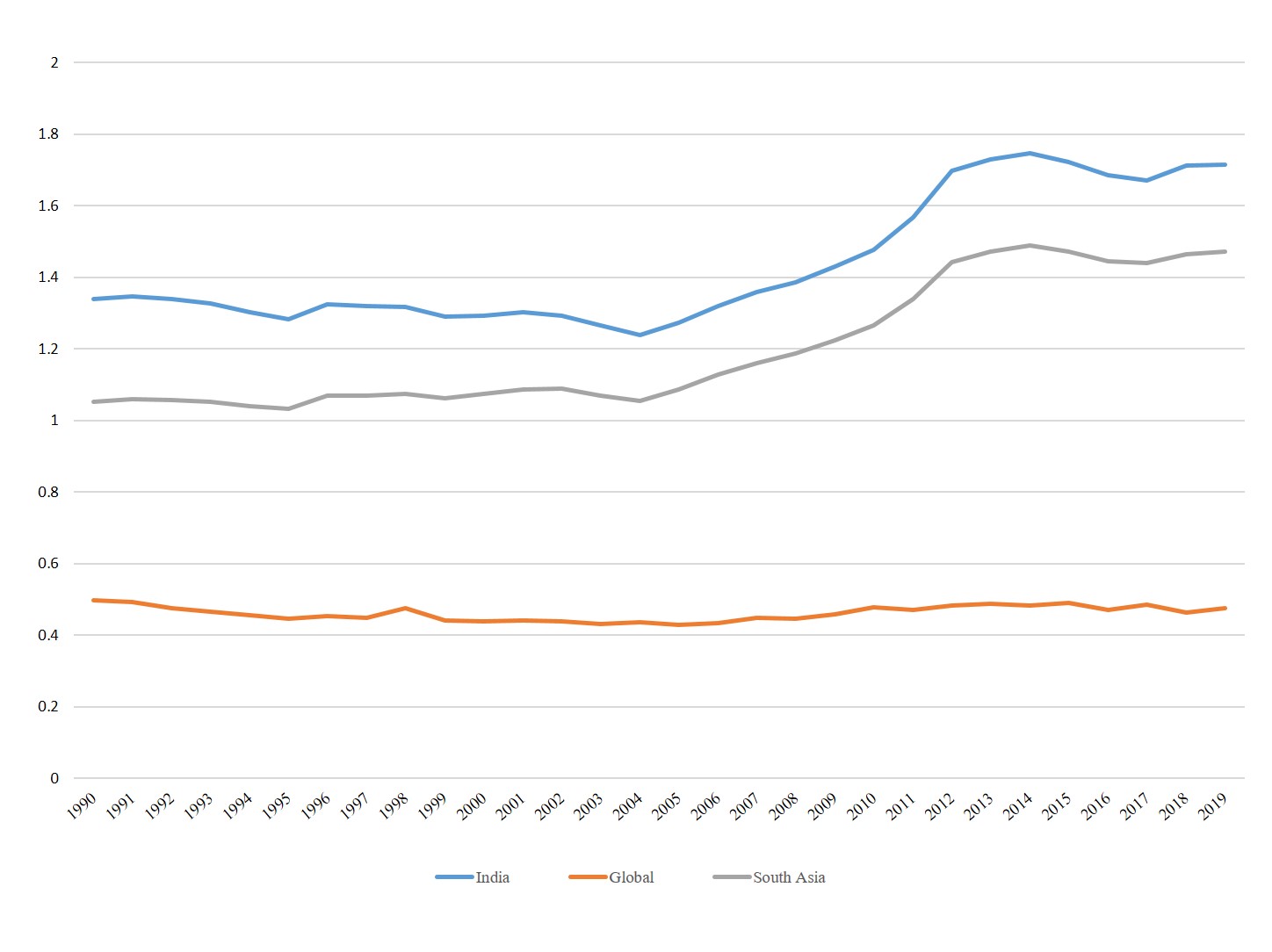
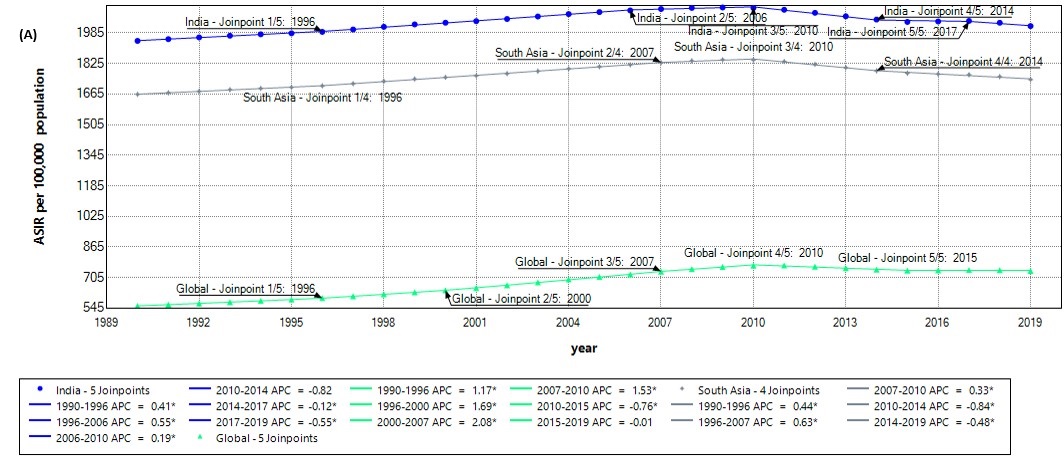
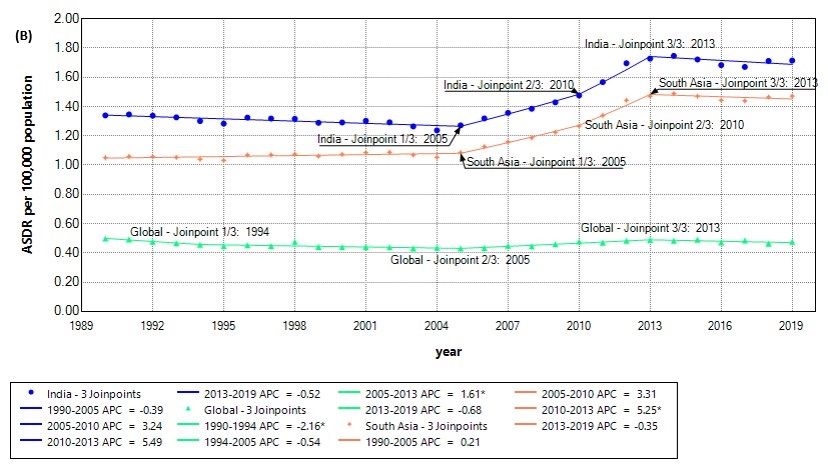
Dengue, a viral infection, has become a significant public health challenge due to the global increase in dengue cases in recent decades. It is estimated that annually, dengue leads to around 390 million infections and about 20,000 fatalities [1]. According to the World Health Organization, nearly 3.97 billion individuals across 128 countries are susceptible to dengue, with an estimated 50 million cases occurring each year [1, 2]. Globally, the incidence of dengue has multiplied nearly eightfold from 1990 to 2019 [3] and 30- fold since the 1960s [4], with considerable geographic expansion and is a pandemic threat in tropical and subtropical regions. During 2000-2015, the deaths due to dengue rose from 960 to 4,032[3]. This surge is attributed to factors like rapid urbanization, climate change, and increased international travel, all of which create favorable conditions for the Aedes mosquito vectors that transmit the virus. Bhatt et al. found its ubiquitous presence in the tropics, with significant local variations attributable to factors such as rainfall, temperature, and urbanization[1]. Their findings suggested a far higher number of dengue infections globally than previously estimated by the World Health Organization, thus redefining the perceived public health burden of dengue. Studies show that the lack of vaccines and insufficient vector control measures, has contributed to the disease's rapid emergence and global spread [1].
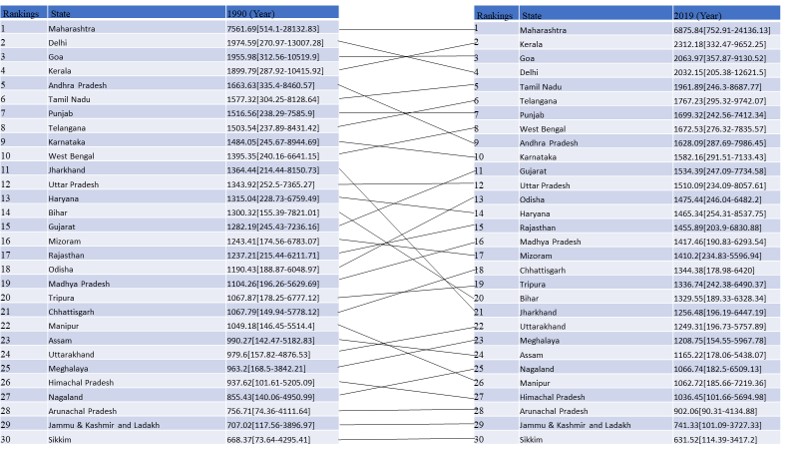
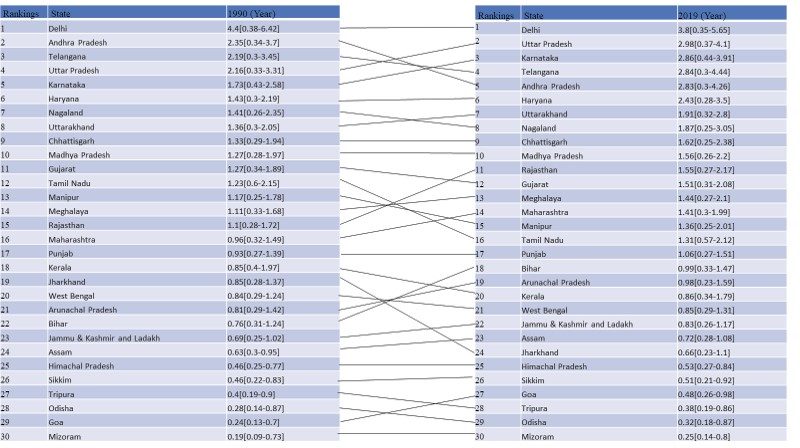
Globally, the distribution and burden of dengue have been a subject of extensive research. A systematic analysis of the global dengue burden from 1990 to 2017, revealed a significant increase in both the incidence and mortality associated with dengue [5]. This increase, coupled with variations in socio-demographic indices, suggests that has varying impacts across different regions and socio-economic contexts highlighting its spread at a global level. Gubler discussed the dramatic increase in these diseases over the past two decades, attributing the resurgence to a combination of ecological, environmental, and sociodemographic changes [2]. This trend is particularly alarming in India, a country with a long history of dengue outbreaks.
Dengue is characterized by its complex transmission dynamics, which involve interactions among the host, the vector, and the virus, and are significantly influenced by environmental and climatic factors [2, 4]. Mutheneni et al. underscored the variability in extrinsic incubation period (EIP) across diverse climatic conditions, which in turn affects regional dengue risk in different climatic zones of India [4]. For instance, the state of Kerala demonstrated a notably faster EIP during the monsoon period, correlating with increased dengue cases. Such findings emphasize the necessity for climate-specific disease forecasting models in dengue-prone areas.
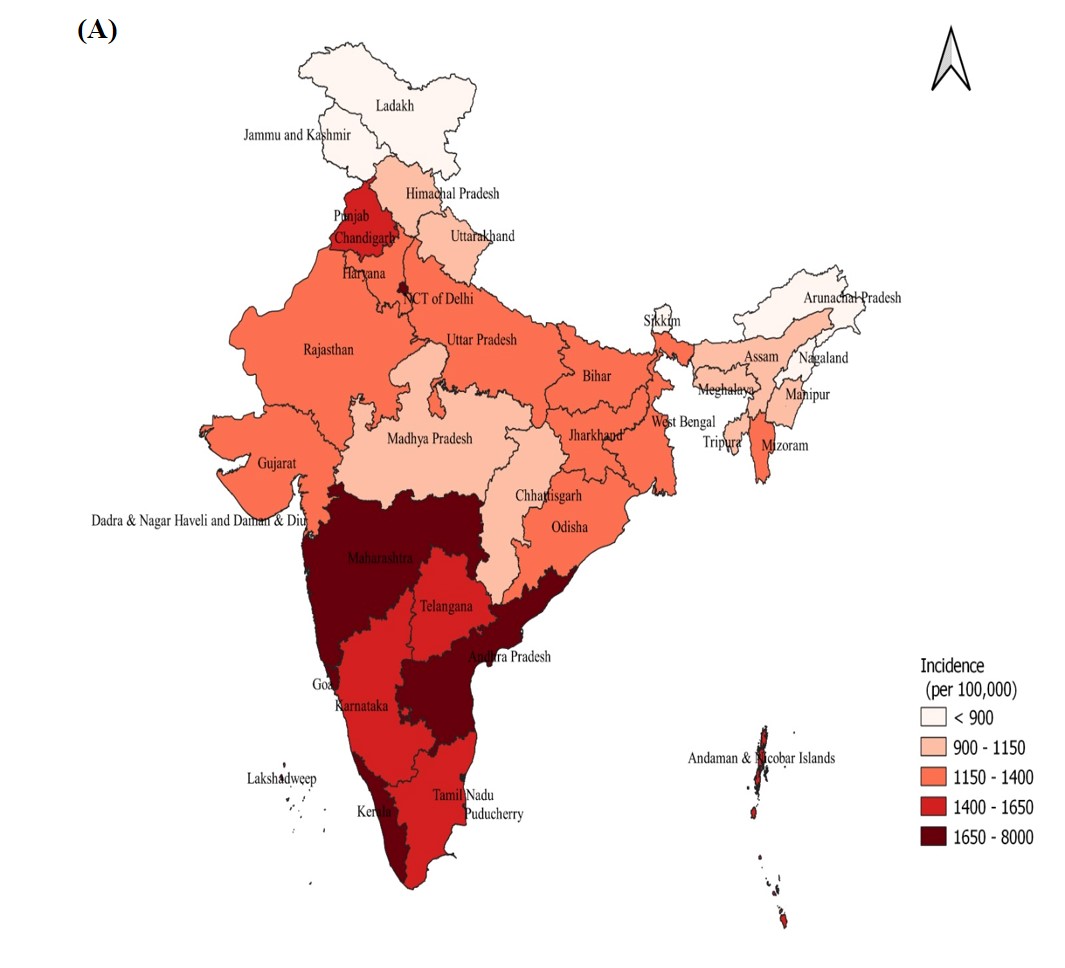
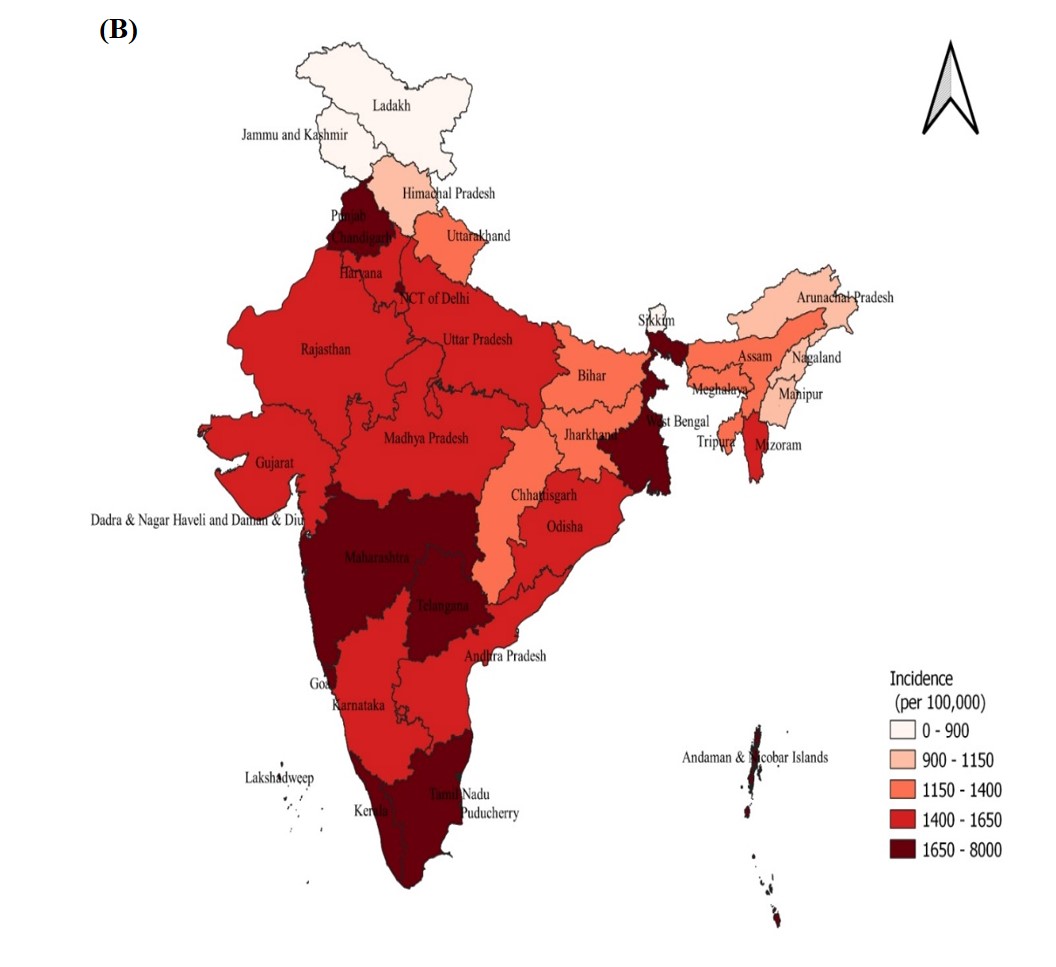
The quantification of dengue infection load in different parts of India is limited. The burden of dengue infection across geographical regions of India is poorly quantified[6]. With its dense population and tropical climate, India experiences a substantial burden of dengue cases annually [2] making it a dengue epidemic country. There were 94198 dengue cases in India between January and October 2022 [7]. As to the latest available statistics, there were 110,473 cases of dengue reported in India between January and September of 2023 [8]. The patterns and characteristics of dengue fever in the Indian subcontinent have undergone significant and complex changes over the last sixty years, including variations in dominant strains, impacted regions, and the severity of the illness [9]. Researchers estimated the number of dengue infections to be substantially higher than the figures reported by the World Health Organization [1], underscoring the need for improved surveillance and reporting. This discrepancy points to a potential underestimation of the disease's true burden and highlights the necessity for enhanced disease control strategies.
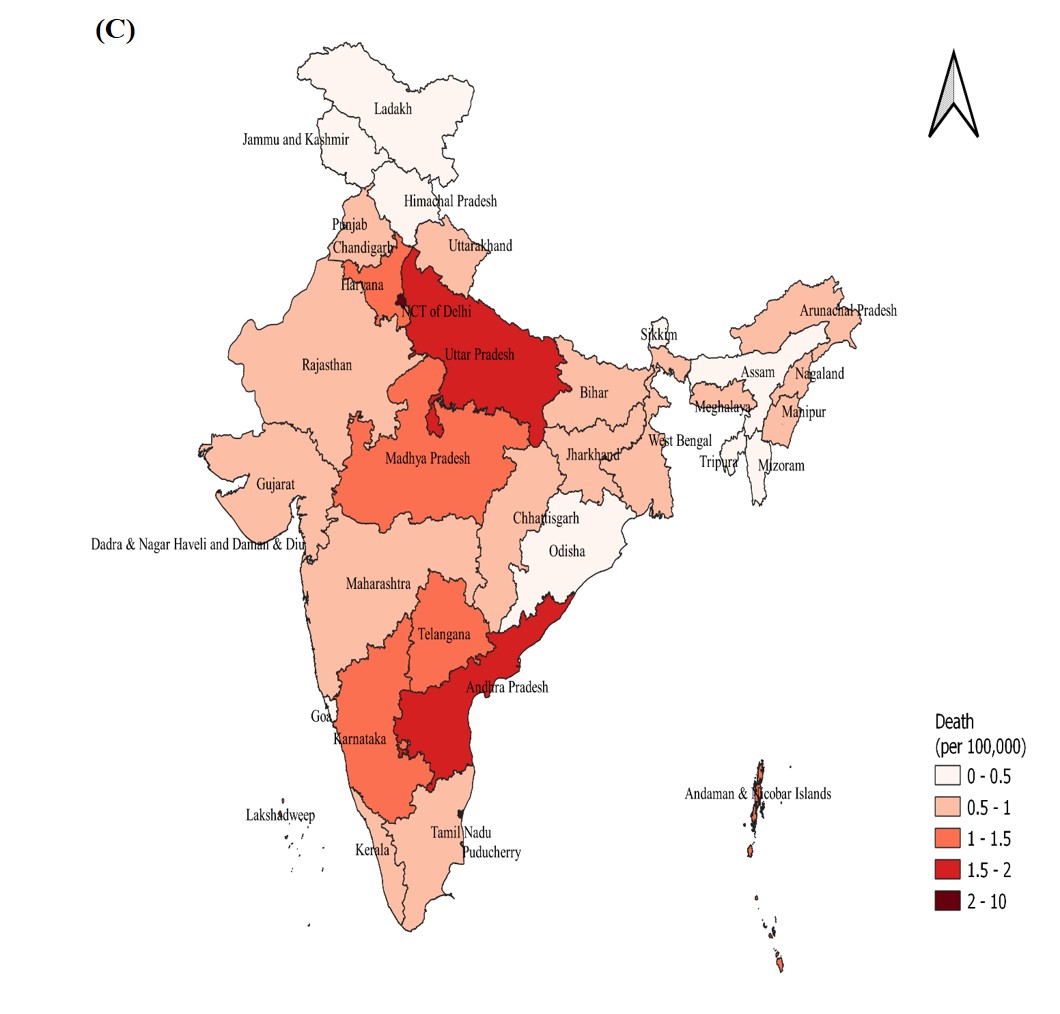
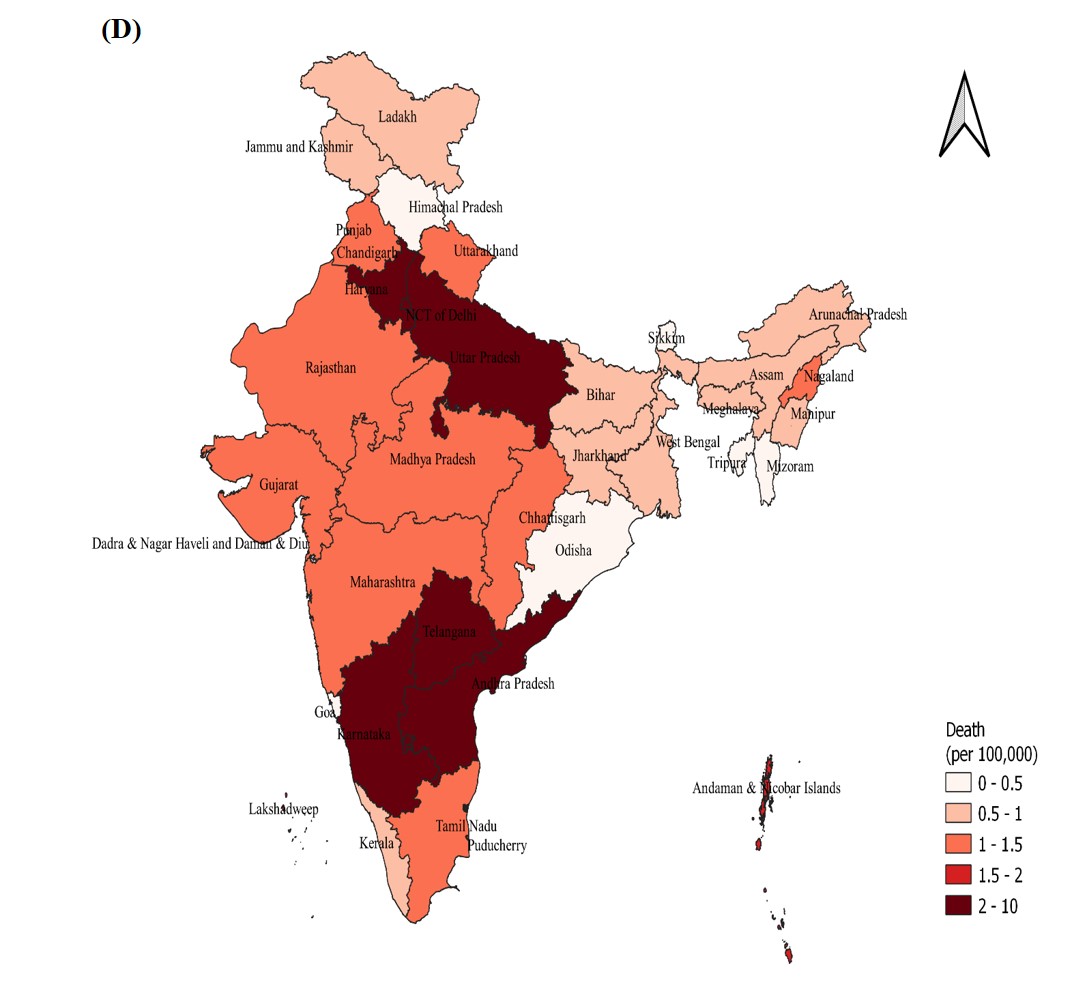
In India, a country with diverse climatic conditions and varying socio-economic environments, dengue presents a significant public health challenge. The burden of dengue infection in India is heterogeneous, with evidence of high transmission in northern, western, and southern regions [6]. The dynamic nature of dengue transmission, geographic heterogeneity influenced by urbanization, climate change, and vector behavior, necessitates an in-depth analysis of temporal trends to understand the evolving epidemiology of the disease. Previous research has often been limited in scope, either geographically or temporally or in standard methodology to capture the regional heterogeneity[6, 7, 9, 10]. This study aims to bridge this gap by providing a comprehensive, long-term analysis at both the national and state levels. Such an analysis is crucial for effective public health planning and resource allocation. By identifying periods and locations of significant changes