for relaxation contribute to elevated stress levels [5]. Collectively, these stressors increase the risk of psychological challenges among medical students, including anxiety, depression, substance abuse, and suicidal ideation.
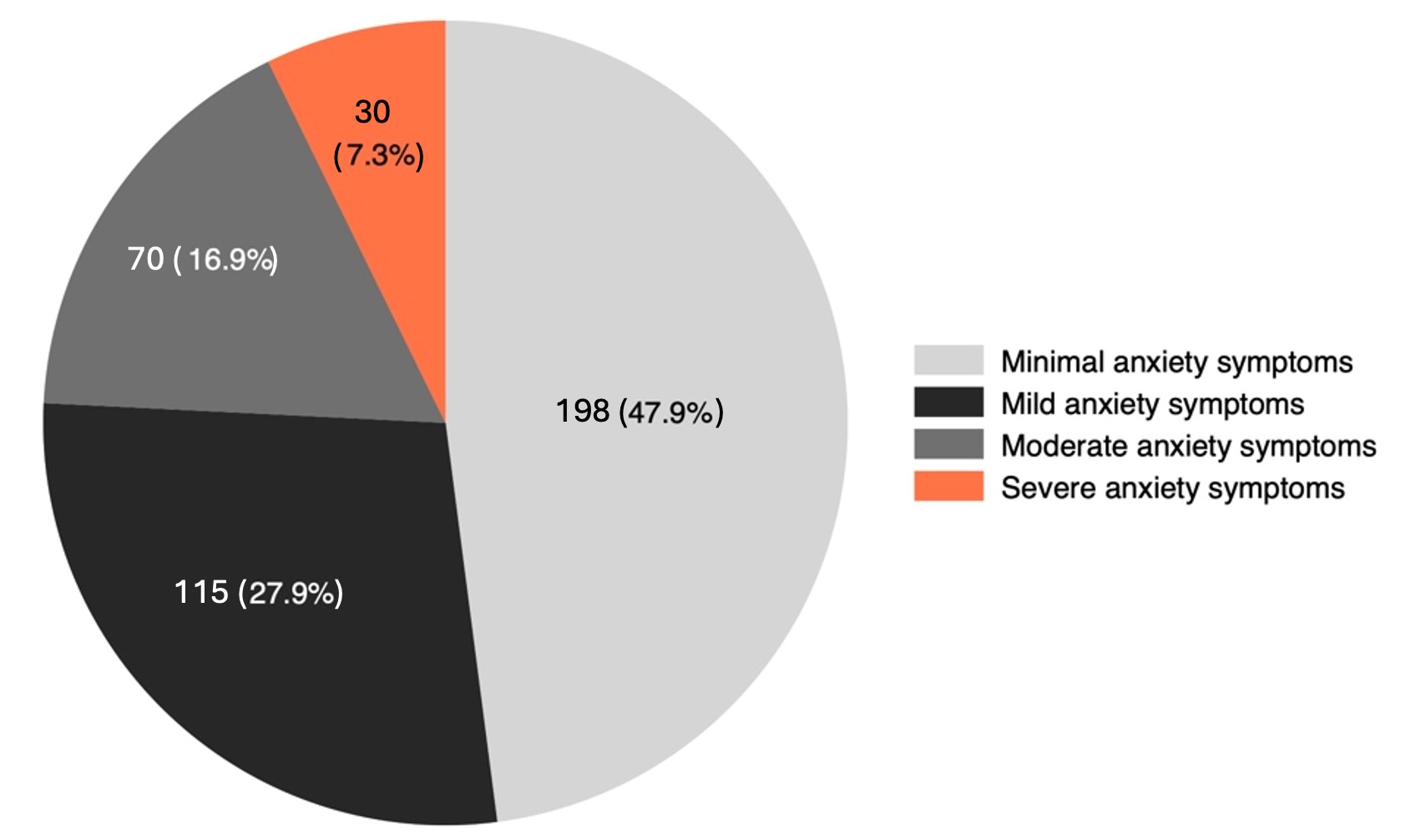
Global studies consistently report a high prevalence of mental health concerns among medical students, with anxiety being one of the most critical issues [6,7]. Approximately one-third (33.8%) of medical students worldwide are affected by anxiety, with even higher rates observed in the Middle East and Asia. A recent systematic review and meta-analysis conducted by Kaur et al. reported the prevalence of anxiety among medical students in India to be 50% (95% CI 42% - 58%) [4]. Evidence suggests that these vulnerabilities often emerge during medical school and, if left unaddressed, can persist into professional practice [8]. These psychological challenges not only impair students' interpersonal relationships and academic performance but also undermine their professionalism and empathy toward patients, potentially affecting the quality of care they provide [9,10].
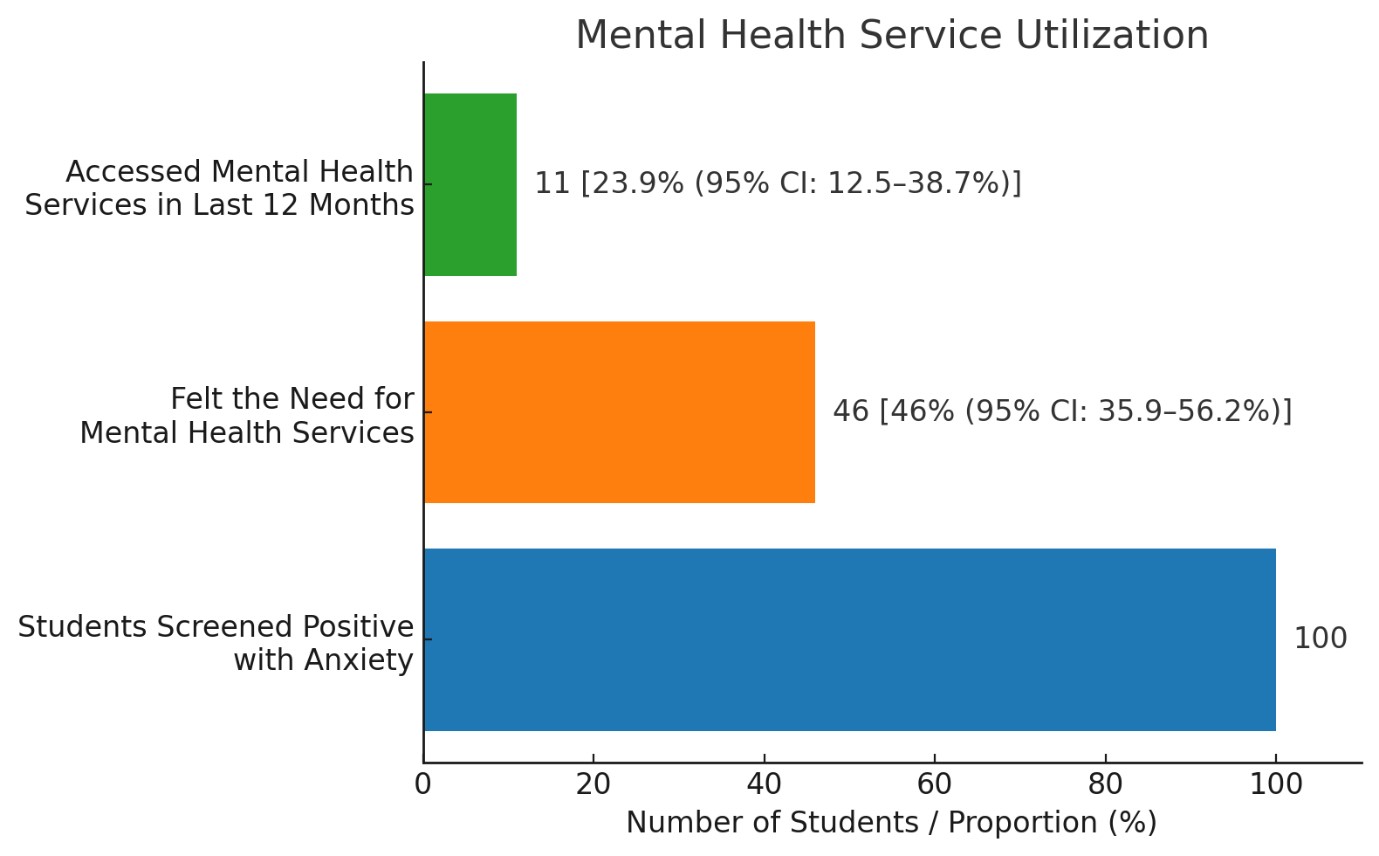
This global burden of anxiety is further compounded in the Indian context, where cultural stigma surrounding mental health and limited access to professional support act as additional barriers to care. Although previous research has identified anxiety as a significant issue among medical students, there are notable gaps in the literature. Most studies focus exclusively on the prevalence of anxiety or its associated factors, with limited attention given to students' perceptions of their mental health needs. Furthermore, the extent to which students access mental health services remains underexplored. Studies have rarely investigated the disparity between the perceived need for mental health care and actual service utilization, leaving critical questions unanswered about the unmet needs in accessing mental health support.
The primary objective of this study is to estimate the prevalence of anxiety among undergraduate medical students. Additionally, it aims to identify the sociodemographic, academic, and lifestyle factors that are associated with anxiety within this population. Furthermore, the study seeks to evaluate the gap between the perceived mental health needs of students and their actual utilization of mental health services.
Methods
Study setting and design
This cross-sectional study was conducted at a medical college in New Delhi, India, during June 2023. The study aimed to estimate the prevalence of anxiety among undergraduate medical students and identify associated factors.
Study participants
Undergraduate medical students from all semesters enrolled in the MBBS program at the institution were invited to participate. Inclusion criteria required students to provide written informed consent, while students under the age of 18 and those who did not give consent were excluded from the study.
Sample size and sampling method
The sample size was calculated to be 430 students, based on a prevalence of anxiety of 20.2%, with a 4% absolute error and a 10% non-response rate [11]. A list of all enrolled students was obtained, and each was assigned a unique serial number. Simple random sampling was employed using computer-generated random numbers to select participants. Students who could not be contacted after three attempts were classified as non-responders.
Study tools
Data collection for the study was conducted using a structured, self-administered questionnaire designed to gather comprehensive information on various aspects relevant to the research objectives. The questionnaire included three main sections. The first section captured sociodemographic details such as age, gender, academic semester, and other relevant variables. We have used modified Kuppuswamy Scale 2023 to assess for socio-economic status [12]. The second section focused on screening for anxiety using the GAD-7 scale, a validated and reliable tool widely